“Therepi” device attaches directly to the damaged heart, enabling delivery of medicine from a port under a patient’s skin to augment cardiac function.

After a patient has a heart attack, a cascade of events leading to heart failure begins. Damage to the area in the heart where a blood vessel was blocked leads to scar tissue. In response to scarring, the heart will remodel to compensate. This process often ends in ventricular or valve failure.
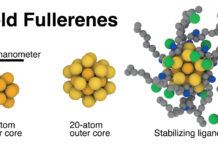
A team of researchers is hoping to halt the progression from heart attack to heart failure with a small device called “Therepi.” The device contains a reservoir that attaches directly to the damaged heart tissue. A refill line connects the reservoir to a port on or under the patient’s skin where therapies can be injected either by the patient or a healthcare professional.
A new study published in Nature Biomedical Engineering involving a team of researchers from MIT, Harvard University, Royal College of Surgeons in Ireland, Trinity College Dublin, Advanced Materials, and BioEngineering Research (AMBER) Center and National University of Ireland Galway details how Therepi can be used to restore cardiac function.
“After a heart attack we could use this device to deliver therapy to prevent a patient from getting heart failure,” explains Ellen Roche, co-first author of the study and assistant professor at MIT’s Department of Mechanical Engineering and Institute for Medical Engineering and Science. “If the patient already has some degree of heart failure, we can use the device to attenuate the progression.”
Two of the most common systems currently used for delivering therapies to prevent heart failure is inefficient and invasive. In one method, drugs are delivered systemically rather than being administered directly to the site of the damage. The volume of drugs used has to be limited to avoid toxic side effects and often only a small amount reaches the damaged heart tissue.
“From a pharmacological point-of-view, it’s a big problem that you’re injecting something that doesn’t stay at the damaged tissue long enough to make a difference,” says William Whyte, co-first author and PhD candidate at Trinity College Dublin and AMBER.
Read more: A new way to mend a broken heart
thumbnail courtesy of mit.edu