Evolving strains of multi-drug resistant pathogens are a growing global concern, outpacing drug discovery efforts and undermining the efficacy of existing antibiotics. The development of comprehensive diagnostics for clinical applications will become crucial to control escalating health risks. Existing laboratory tests to diagnose infectious disease are generally carried out via culture-based methods that usually take days to generate results. Rapid molecular diagnostic tests can comparatively identify microbial nucleic acids (NA) in clinical samples directly in less than an hour with nucleic acid amplification tests (NAATs). Existing NAATs are, however, limited by inadequate levels of multiplexing (i.e. the number of strains or sequences detected in a single reaction) and inaccuracies with detecting mutations.
Scientists and engineers recently collaborated to develop a fully integrated, miniaturized semiconductor biochip with closed-tube detection chemistry to perform multiplexed NAAT with aims to overcome existing limitations. The system can rapidly amplify DNA and RNA sequences in a single sample, including species signatures, genotypes, and mutations that confer pathogenic drug resistance. Feasibility of the system was first demonstrated by identifying and quantifying multiple viral RNAs and DNAs from respiratory tract pathogens. Subsequently, the system was used to detect > 50 antibiotic-resistant mutations across multiple genes of the Mycobacterium tuberculosis (MTB) genome. The research is published in Nature Biotechnology.
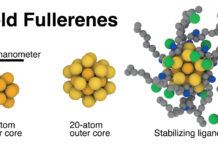
In the study, Hassibi et al. designed and developed a miniaturized and single-use (disposable) semiconductor, using conventional sub-micron, complementary metal oxide semiconductor processors (CMOS). The architecture of the biochip contains a fluid chamber with thermocycling capabilities and DNA capture probes with fluorophores that sit above an embedded biosensor array. The fluid chamber of the system can receive multiplex PCR reagents and microbial nucleic acid of a clinical pathogen – with a specific region of interest responsible for drug resistance—for its amplification. When the amplified region of the microbial genome is in close affinity to the DNA capture probe on the biochip, individual biosensor pixels will be activated to detect and differentiate between the wild-type and mutant microbial strains.
In the NAAT module, fluidic ports can introduce the multiplex PCR mix and extracted nucleic acids into the chamber for nucleic acid amplification. The biochip houses an array of 32 x 32 biosensing pixels, each with embedded photodiode, heaters, and detectors. The system is built to identify multiple and distinct nucleic acid sequences in real-time via the inverse fluorescence transduction (IFT) method. By function, the CMOS biochip can detect real-time IFT signals while controlling the temperature of the fluid chamber to enable nucleic acid amplification.
Read more: A miniaturized semiconductor biochip to identify drug-resistant pathogens
thumbnail courtesy of phys.org